







Reveleer Risk Adjustment Platform
A redesigned AI-powered health plan platform that leverages NLP and streamlined workflows to extract diagnoses from unstructured medical records, enhancing efficiency and improving productivity for clinical abstractors.
Role
Product Designer
Timeline
Oct 2024 - Apr 2025
Team
1 Director of Experience
1 Product Designer
1 UI Illustrator
Stakeholder
Product Managers (Clinical / Ai )
Engineers (NLP / Front-end / QA)
Clinical Innovation Lead
Customer success manager
Tool
Figma
UserTesing.com
Jira
IMPACT
40%
Increase in Reimbursement
More accurate diagnosis coding boosted RAF scores, helping health plans earn 40% more reimbursement per patient chart.
30%
More Efficient Workflows
Streamlined collaboration between clinical coders and reviewers, saving thousands of manual review hours.
1.2M
High-Volume Processing
1.2M patient charts processed in 4 months with AI (NLP), accelerating review efficiency
+6.8
NPS growth in one year
Customer satisfaction rose from 31.7 (Q2 2024) to 38.5 (Q2 2025), reflecting stronger usability and outcomes.
PROCESS

INTRODUCTION
What does Reveleer do?
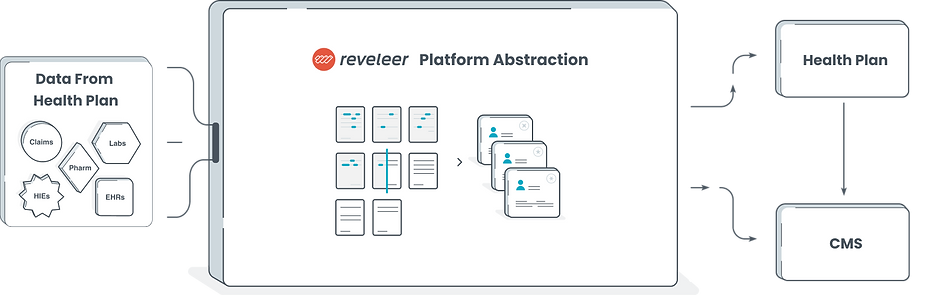
Reveleer is an AI-powered platform that helps health plans manage the full lifecycle of risk adjustment — from medical record review to diagnosis capture and data submission for government reimbursement.
Platform Customers (Health Plan Companies)



Data In, Value Out:
The Reveleer platform ingests structured and unstructured health data, applies AI to extract and validate diagnoses, and generates risk-adjustment submissions for health plans and CMS (Centers for Medicare & Medicaid Services).
What does Risk Adjustment Data Entry involve?
In risk adjustment, Data Entry refers to the process of reviewing unstructured clinical documents, validating diagnoses, and accurately coding them to calculate a member’s RAF (Risk Adjustment Factor) score.
Within Reveleer’s end-to-end platform lifecycle, Data Entry is a core function that directly impacts the accuracy and completeness of data submitted to health plans and CMS (Centers for Medicare & Medicaid Services). It plays a critical role in ensuring that diagnoses are properly captured and reimbursed — ultimately supporting financial accuracy and regulatory compliance for our customers.

UNDERSTANDING
Business Goal

Enable health plans to secure accurate and efficient government reimbursement at scale.
Product Goal

Optimize the Data Entry workflow through improved interaction design to boost coding productivity, accuracy, and usability.
Who Are Our Users
A team of clinical coders responsible for reviewing unstructured medical records and accurately assigning diagnosis codes that directly impact government reimbursement. Most have prior experience as registered nurses or clinical professionals and are trained in risk adjustment and medical coding standards like HCC and ICD-10.

Problems
1. Lack of task clarity and workflow guidance
Clinical coders struggled to understand what to do next, leading to low confidence and inefficient decision-making.
2. Low productivity from redundant coding
Coders had to assign identical ICD codes one by one across encounters within the same HCC category, resulting in repetitive work and slower throughput.
3. Disorganized interface with visual noise
Poor hierarchy, color misuse, and excessive clicks made the experience cognitively taxing and frustrating.
4. High training burden
Inconsistent interactions and vague feedback loops required extensive onboarding and manual coaching.

OPPORTUNITIES

Prioritized worklist and in-app onboarding guidance.

NLP capture and multi-select validation eliminate redundant coding across related diagnoses.

Modernized the UI to improve clarity, accessibility, and workflow efficiency.

Added annotations and history review to give users full context, strengthening feedback loops and improving team communication.
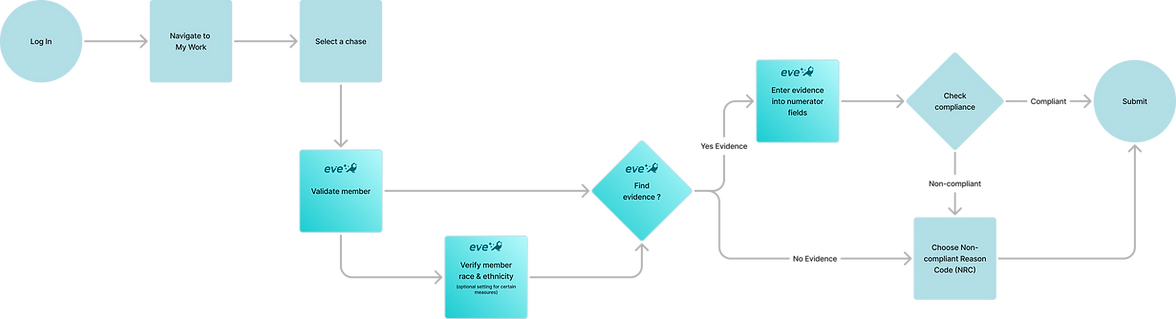
AI Opportunity — How EVE Accelerates the Workflow
AI (EVE) accelerates the abstraction workflow by replacing the most manual, repetitive steps with intelligent automation. Instead of coders searching, validating, and entering information themselves, AI (EVE) now detects relevant evidence, pre-populates fields, verifies member details, and assists with compliance decisions.
Note:
All patient information in this mockup is fictitious and used solely for demonstration, in compliance with HIPAA privacy standards.


Final Design
Old Welcome Page ( Risk 2.0 )
Missing work queue and performance overview made it difficult for coders to understand daily assignments or track goals.
Important buttons were not visually prominent.
Illustrations felt outdated and lacked clear functional cues
New Version
New Welcome Page ( Risk 3.0 )
A prioritized work queue, real-time performance insights, and a modern, accessible UI help coders clearly understand their task order, stay focused, and stay productive.
The built-in Help Center provides quick access to domain knowledge — reducing time spent on training and support.
Built-In Onboarding
A guided onboarding experience helps new coders ramp up faster — cutting training time, lowering costs, and boosting early productivity.

Old Data Entry Page ( Risk 2.0 )
Poor visual hierarchy made the page cluttered and hard to navigate.
Key tabs were placed at the bottom, breaking expected user behaviors.
Users had to open and click through each card manually, slowing down the process.
Hidden task priorities made key functions hard to identify and workflows difficult to follow.
New Version
Flexible & Efficient Layout
The new layout is flexible and scalable — coders can resize panels and work across dual screens for better focus and efficiency. Familiar Material icons make interactions more intuitive, reducing the learning curve.
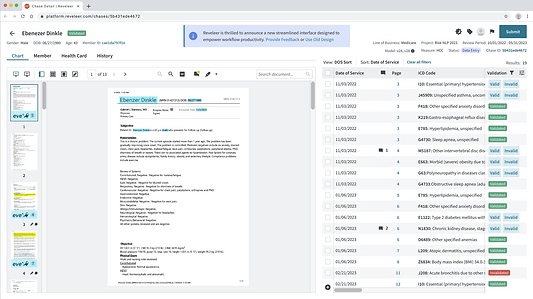
Diagnosis Table View
In the previous version, each diagnosis was buried inside collapsible cards, requiring coders to open and validate them one by one, which is a slow and repetitive process.
The redesigned UI introduces a table-based grid view that displays all diagnoses upfront.
Coders can now:
Multi-select diagnoses to validate or apply VRC codes in bulk
Use filters to prioritize their work by date, condition, or status
Switch view modes to match different workflows


Old Ai Evidence Capture ( Risk 2.0 )
Evidence and coder highlights shared the same color, causing visual confusion.
Without a centralized view, coders had to scroll to find scattered evidence, making validation slow and inefficient.
New Version
New AI-Powered Evidence Capture (Risk 3.0)
Our Evidence Validation Engine (EVE) uses OCR and NLP to extract diagnoses and highlight supporting evidence from medical charts. The new UI introduces visual thumbnails and multiple view modes, enabling coders to quickly locate AI-validated evidence. Clickable thumbnails take users directly to the source page—saving time and streamlining validation.
HCC Card for Smarter Validation
Centralizes a member’s diagnosis history by HCC category, making it easy for coders to review past validations, avoid duplication, and ensure consistent, accurate coding.
Comprehensive History Page
The history page brings together every action, from data upload to final submission, including status updates and task assignments, providing coders with complete visibility into the patient’s history and the full workflow.
TAKEAWAYS
Design systems enable scalable impact
Standardized components reduce complexity, improve consistency, and make platforms easier to scale—especially in regulated industries like healthcare.
Cross-functional collaboration is essential
Working closely with engineers, PMs, and domain experts ensured designs were feasible, aligned, and rooted in real workflows.
Data drives better design decisions
Quantitative and qualitative data helped validate patterns, surface pain points, and shape resilient, user-centered solutions.
Accessibility builds lasting products
By following WCAG guidelines, I created designs that were inclusive, sustainable, and regulation-compliant.

Domain knowledge empowers smarter UX
Understanding healthcare and health plan workflows and terminology allowed me to design with confidence and clarity in a highly complex space.
If you have any questions or would like to see the full project, reach out at liuyixing1018@gamil.com

Behind the Collaboration



